For years, prior authorization (PA) has been a symbol of healthcare’s administrative drag. Providers fax requests, chase approvals, and wait days—or weeks—for decisions. Patients, meanwhile, bear the cost of delay: disrupted treatment plans, postponed surgeries, and in some cases, preventable harm.
That status quo will not survive 2026.
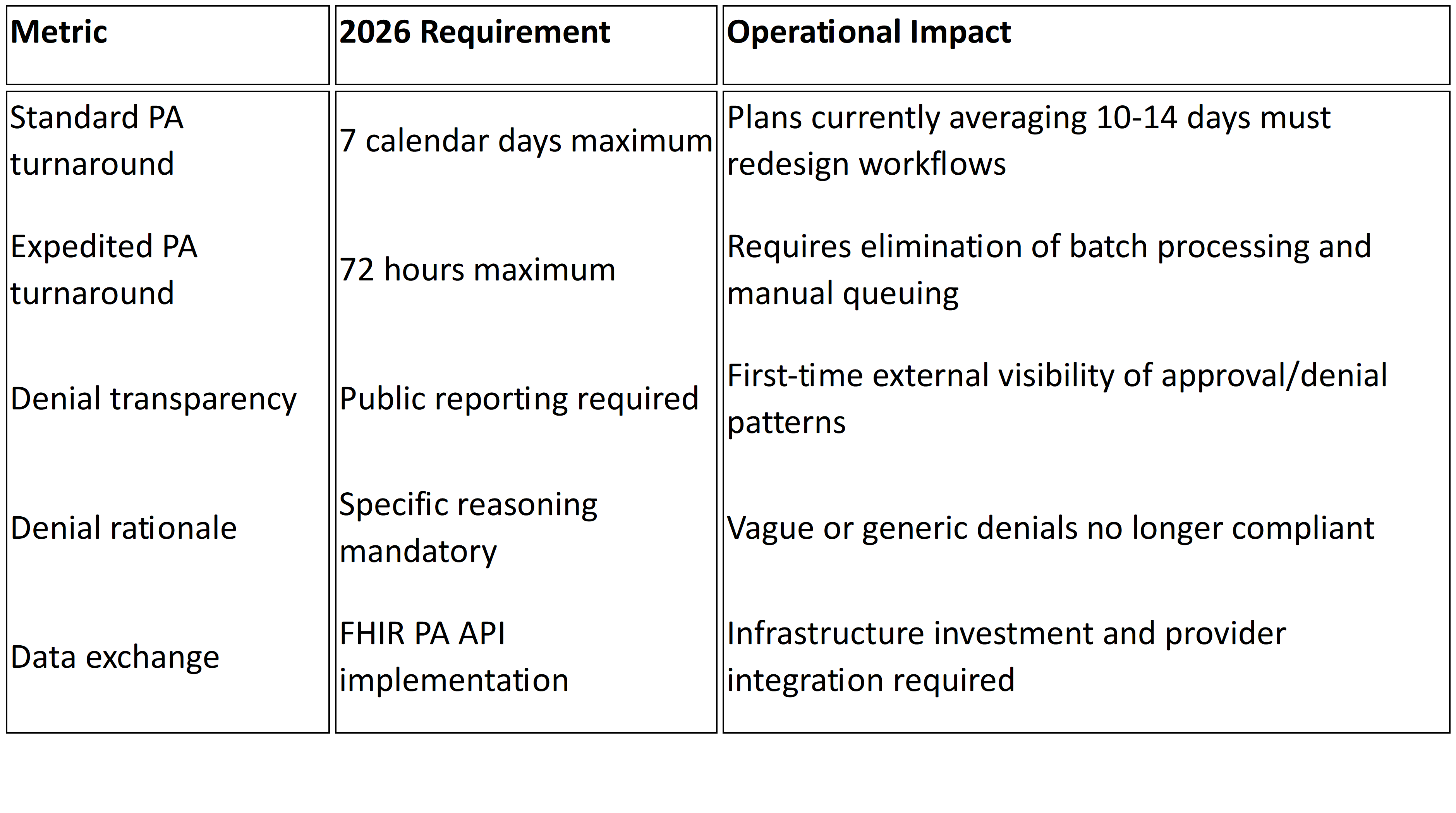
Under CMS’s Interoperability and Prior Authorization Final Rule (CMS-0057-F), payers must meet strict turnaround standards: urgent requests decided within 72 hours, and standard ones within seven calendar days. For an industry accustomed to workflows that stretch far beyond those timelines, this represents a fundamental shift. The countdown has begun.
What’s Really at Stake
At its core, the new mandate is about more than speed. It’s about rebalancing the relationship between patients, providers, and payers. Physicians have long argued that PA undermines clinical autonomy and delays necessary care. Nearly 90% of physicians say prior authorization leads to care delays, and more than one in four report that it has led to serious adverse events—including hospitalizations.1
By imposing the 72/7 standard, CMS is forcing payers to move from reactive, paperwork-heavy systems to real-time, digital workflows. Failure to adapt is not just a compliance risk—it’s a reputational one. Every denial, every delay, and every approval rate will soon be publicly visible. Members and providers will know which plans meet expectations and which fall short.
The Operational Challenge
For payers, the challenge is not theoretical — it’s operational. Prior authorization remains one of the most resource-intensive processes in healthcare, requiring armies of staff and expensive workflows to manage intake, clinical review, documentation, and appeals. Large national plans process millions of requests annually, with even modest inefficiencies magnified at scale into significant costs and compliance risks.
Recent analysis underscores the stakes. According to The Costly Lever of Prior Authorization, the average manual PA transaction costs payers $3.52 each; however, a fully electronic PA transaction costs a payer $0.05.2 Multiplied across tens or hundreds of thousands of PAs per year, that difference becomes millions in needless administrative spend. Meanwhile, a Milliman study in Massachusetts estimated that reducing or eliminating PA for certain services could meaningfully reduce allowed costs for payers in commercial and Medicaid markets.3
The interlocking challenges can be summed up as:
- Volume at scale — Processing millions of requests annually means even small workflow delays or manual-intensive steps can push plans past CMS’s 72-hour and 7-day limits, or inflate admin costs significantly.
- Complexity of cases — Many requests require extensive documentation across multiple systems; manual routing, appeals, and follow-ups add both time and cost.
- Transparency pressures — Starting in 2026, plans must not only meet deadlines but also publish performance data. Missed timelines or unclear denials will quickly erode trust with regulators, providers, and members. Public reporting would also expose costs and inefficiencies to scrutiny.
In other words: compliance with the rule is table stakes. Execution — at speed, at scale, and under public scrutiny — is existential.
Technology Is Necessary, but Not Sufficient
The 72/7 mandate is often framed as a technology problem: build APIs, adopt FHIR standards, automate intake. And while these are critical, technology alone won’t close the gap. The deeper challenge is aligning people, processes, and policy around new ways of working.
Consider intake. Optical character recognition (OCR) can digitize clinical documents, and natural language processing (NLP) can extract relevant details. But unless review workflows are redesigned to integrate those insights—triaging straightforward cases for auto-approval, surfacing complex ones for clinical review—the gains will be marginal.
Similarly, APIs enable real-time data exchange, but if provider portals remain clunky or staff training is neglected, friction will persist. As with most transformations, the bottleneck is rarely the tool. It’s the adoption.
The Strategic Imperative
The countdown to 72/7 is more than a compliance deadline; it’s a strategic forcing function. Plans that embrace it can reposition themselves as faster, more transparent, and more provider-friendly. Those that resist risk being labelled as laggards in a market where provider trust is already fragile.
The logic is straightforward:
- Faster approvals reduce provider friction, leading to stronger networks and fewer out-of-network escalations.
- Clear, consistent denials minimize appeal rates and litigation risk.
- Transparent performance reporting builds member confidence at a time when health plan trust lags behind most other industries.
Seen through this lens, the rule is not just a regulatory burden. It’s an opportunity to differentiate.
Turning Deadline into Advantage
So how can payers get from here to 2026 without stumbling? The path forward involves four priorities:
- Automate intake at scale – Replace manual data entry and faxes with OCR, NLP, and API-driven submissions. Free staff to focus on clinical judgment rather than paperwork.
- Embed clinical intelligence – Use AI/ML models to summarize records, flag missing information, and suggest next steps. Ensure final decisions remain clinician-led but accelerated.
- Redesign workflows – Build parallel processing models that can handle both high-volume routine cases and complex exceptions without bottlenecks.
- Invest in transparency tools – Create dashboards to track turnaround times, denial reasons, and approval rates in real time—before CMS and the public do.
Plans that integrate these capabilities will not only meet CMS deadlines but also reduce administrative waste, strengthen provider relations, and improve member experience.
The Bottom Line
The 72/7 mandate is coming fast. By January 2026, every payer will be judged not just by regulators but by the providers and patients who experience the impact of their decisions. Compliance will be visible. Delays will be public. And excuses will no longer be tolerated.
The question for payer CEOs is not whether they can meet the letter of the rule. It’s whether they can seize the spirit of it—to turn regulatory pressure into strategic advantage.
At Mizzeto, we help payers do exactly that. Our platform combines intelligent intake automation that cuts manual review times with clinical AI integration that surfaces the right insights for faster, more accurate decisions. We also build real-time dashboards that track turnaround performance against CMS benchmarks, ensuring plans don’t just meet the 72/7 mandate but prove it with data. From streamlining utilization management workflows to enabling secure, scalable data exchange, our solution OS designed to move payers beyond compliance into true operational advantage. The 72/7 clock is ticking. The time to act is now.