The Problem Hiding in Plain Sight
For health plans, few operational bottlenecks are as quietly persistent—and costly—as prior authorization (PA) intake. Every day, thousands of requests pour in through fax, email, portals, and clearinghouses. Yet despite the sophisticated systems built to handle medical necessity review, authorization routing, and compliance tracking, the starting point of it all—the intake process—is often neglected.
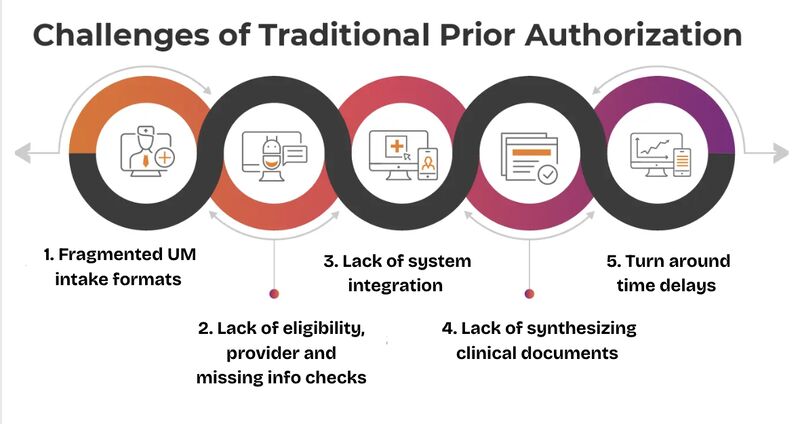
The reality is that many health plans still rely on fragmented, manual workflows to manage the flood of prior auth submissions. Intake teams are stuck toggling between scanned PDFs, legacy document management systems, outdated provider rosters, and multiple eligibility files just to determine if a request is complete and processable. The result is a slow, error-prone, resource-intensive gatekeeping function that delays care, frustrates providers, and drives up administrative overhead.
Ironically, most plans don’t struggle because they lack infrastructure. They struggle because their infrastructure was built to handle review—not to parse and process messy, unstructured incoming data. The core systems weren’t designed for the intake chaos of 2025, where information arrives in every format imaginable, and basic data like member ID, provider NPI, and service codes often require interpretation before integration.
This intake inefficiency sits upstream from every subsequent step—and yet it’s rarely prioritized. Why? Because fixing it has traditionally meant either adding manual labor or undertaking a high-risk replacement of core utilization management platforms. Neither path is attractive to CIOs or COOs already managing legacy migrations and regulatory deadlines.
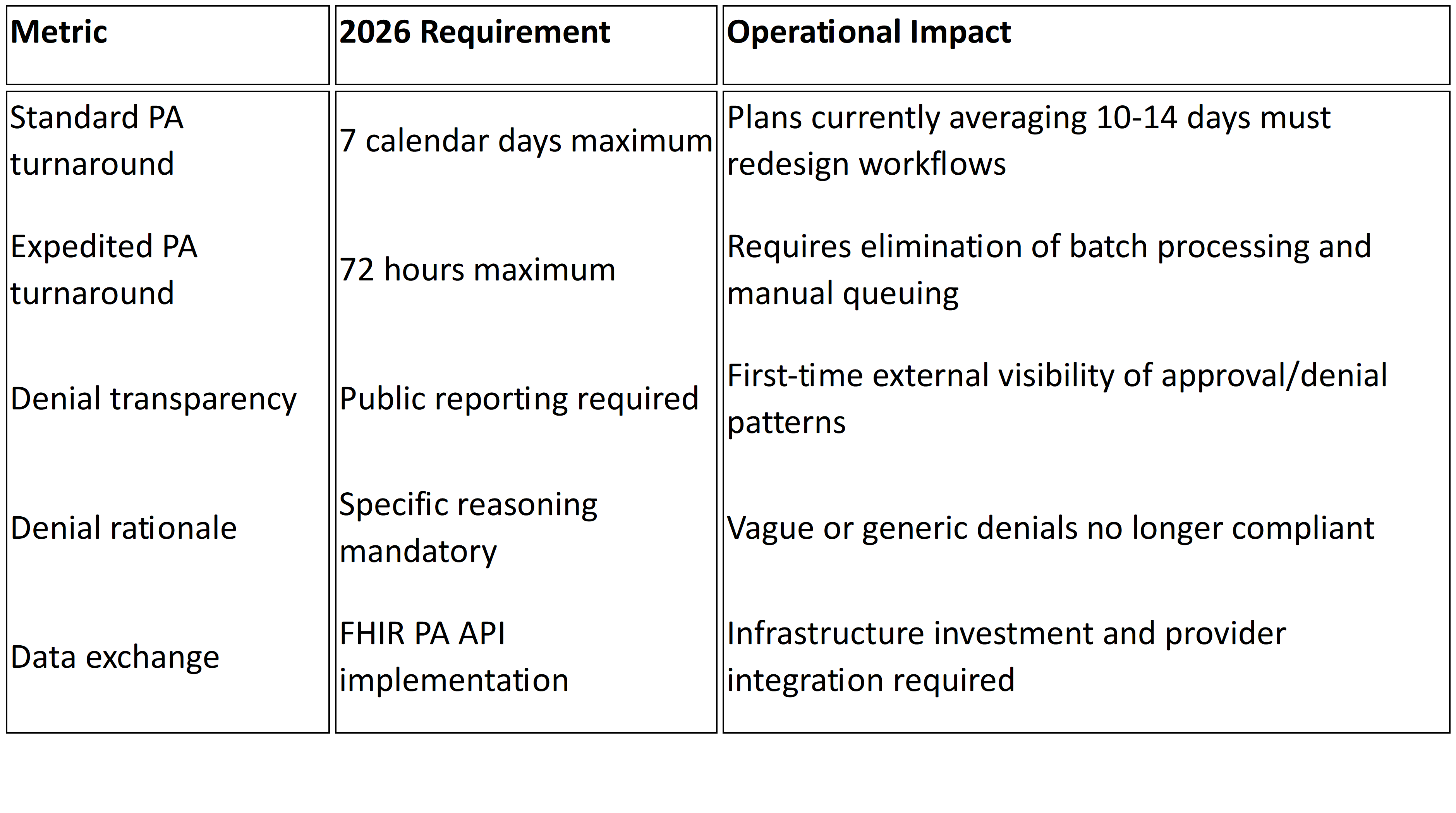
But the cost of inaction is growing. With CMS’s 2026 Prior Authorization mandate (CMS-0057-F) tightening turnaround windows and requiring electronic PA capabilities, intake can no longer be treated as a clerical function. It’s the new front line of compliance and performance.1
Why Intake Inefficiency Is a Strategic Liability
While the pain of prior authorization delays is felt most acutely by providers and patients, the underlying operational burden falls squarely on health plans. When intake is slow or inconsistent, it doesn’t just delay care—it ripples downstream into nearly every facet of plan operations.
Incomplete or misrouted requests lead to longer turnaround times, increased denial rates, and a surge in resubmissions. Nurses are pulled away from clinical review to correct simple data entry issues. Providers call in to clarify missing details. Members wait longer for procedures or medications to be approved. And compliance risks mount as aging requests near regulatory deadlines.
According to the CAQH 2023 Index Report, manual prior authorization costs $13.40 more per transaction than its electronic counterpart, largely due to intake and rework inefficiencies . Yet over 88 million prior auths are still processed manually each year, with 80% of them initiated by fax or unstructured forms.2
Meanwhile, a 2022 American Medical Association survey found that 93% of physicians report care delays due to prior authorization, with 34% citing serious adverse events tied to those delays . The bulk of these delays are not caused by clinical complexity but by administrative friction at intake.3
This creates a strategic liability. Health plans are under increasing pressure to reduce administrative spending (which accounts for 15–25% of total expenditures) while improving provider experience and regulatory compliance . But none of those goals are achievable if the intake function remains slow, manual, and error-prone.4
The real cost isn’t just in labor—it’s in opportunity. Health plans are investing in automation, AI, and real-time decisioning tools. But these investments won’t yield full returns if they’re fed by an intake process that can’t reliably deliver clean, structured, validated data to downstream systems. In effect, sophisticated engines are being starved of usable fuel.
The Solution: Modernizing Intake Without Starting Over
The good news is that fixing PA intake doesn’t require a full rip-and-replace of your core UM system. In fact, the most effective path forward is often modular: implementing intelligent intake layers that sit alongside and integrate with your existing systems, without disrupting what already works.
This modern intake model starts with intelligent document processing. Using OCR tailored for healthcare forms, NLP trained on clinical data, and AI-powered classification engines, health plans can automatically extract structured information from scanned faxes, PDFs, and web forms with high accuracy. These tools go beyond traditional OCR, understanding context and flagging ambiguous or missing data for real-time resolution.
Next comes automated validation. As data is captured, it’s cross-referenced against the plan’s eligibility files, provider rosters, and benefit rules. Does the member exist and is coverage active? Is the provider in-network and authorized? Is the requested service a covered benefit—and does it require prior auth? These checks can now be performed instantly, ensuring only clean, actionable requests proceed to clinical review.
Critically, this new intake layer doesn’t replace your core UM platform. It augments it—feeding clean data into existing workflows, auto-generating work queues, and routing validated requests to the right teams. Most vendors offering intelligent intake solutions provide robust API integrations, ensuring compatibility with legacy systems and allowing gradual rollout across lines of business.
Some health plans are even piloting “zero-touch” intake models, where fully validated requests bypass manual review and move directly to rules-based auto-authorization. While not every case qualifies, even a 20–30% reduction in manual intake workload can deliver measurable ROI within months, according to McKinsey & Company.5
Importantly, these tools also support compliance. By logging when a request was received, when data was validated, and when it moved to review, plans can easily demonstrate adherence to CMS’s forthcoming 72-hour and 7-day turnaround requirements. And because the system ensures eligibility and provider validation before clinical review, the risk of improper denial due to administrative error is dramatically reduced.
Now Is the Time to Act
For health plan leaders, the message is clear: fixing prior authorization starts at intake. And in today’s environment, doing so doesn’t require overhauling your entire system architecture.
The technology exists. The regulatory pressure is building. And the return on investment—lower admin costs, faster approvals, improved provider satisfaction—is compelling. The real question is whether intake modernization will be treated as a strategic imperative or remain buried under more visible initiatives.
C-suite leaders should prioritize intake transformation as a foundational component of digital utilization management. That means investing in tools that turn unstructured faxes and PDFs into structured, validated data. It means automating eligibility and provider checks before clinical review. And it means doing all of this without disrupting the systems your teams already rely on.
As 2026 approaches, health plans that wait to address intake risk falling behind. Plans that act now can turn a persistent bottleneck into a competitive advantage.
At Mizzeto, we help health plans modernize UM intake—without ripping out their core systems. Our intelligent intake suite integrates seamlessly with your existing infrastructure, automating fax, form, and eligibility workflows so your teams can focus on decisions, not data entry. If you're preparing for CMS's 2026 mandate—or simply want to deliver faster care at lower cost—now is the time to act.
Let’s talk about what smarter intake could look like for your organization. Visit www.mizzeto.com or reach out directly to start your transformation.
Sources
1 CMS
2CAQH
3AMA
4Peterson-KFF Health System Tracker