In the age of AI-driven utilization management (UM), one paper trail still refuses to move at the speed of automation: the UM letter.
Whether it’s an approval, denial, or request for additional information, these letters remain the last mile of every UM decision, and too often, the slowest. Despite sophisticated review platforms and integrated medical policy engines, many health plans still rely on legacy templates, fragmented data sources, and manual QA loops to generate what regulators consider a fundamental compliance artifact. UM letters are not just a formality; they are a legal requirement. Under CMS rules, plans must issue timely, adequate notice of adverse benefit determinations, explaining both the rationale and appeal rights to members.
The irony is hard to miss: while decisions are made in seconds, the documentation that justifies them can take days.
The Real Question Behind the Delay
The issue isn’t simply that UM letters take time. It’s why they take time, and what that delay reveals about deeper system inefficiencies.
For health plans, the question isn’t “How can we make letters faster?” It’s “Why are they so hard to get right in the first place?”
A single UM letter must synthesize clinical reasoning, regulatory precision, and plain-language clarity all aligned with CMS, NCQA, and state-specific notice requirements. The challenge is not in the writing, but in orchestrating inputs from multiple systems: clinical review notes, policy citations, benefit text, and provider data.
When those inputs don’t talk to each other, letter generation becomes a bottleneck that slows down turnaround times, increases error risk, and erodes member trust.
Why Templates Must Meet More Than Just Style
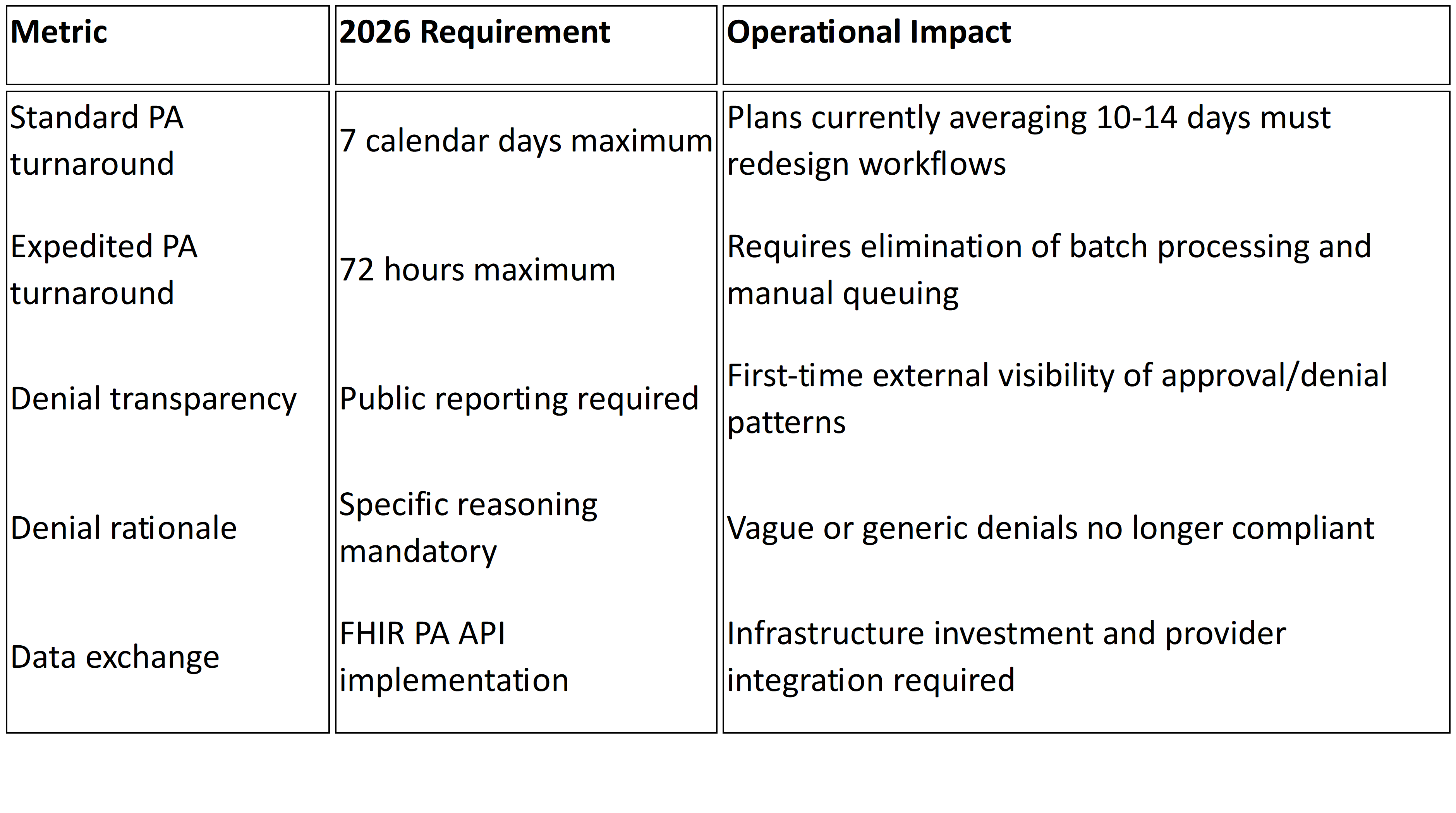
UM letter templates are not just administrative artifacts; they are regulatory documents. Under Centers for Medicare & Medicaid Services (CMS) rules, letters providing notice of adverse benefit determinations must meet detailed content and timing standards. For example, the regulation at 42 CFR § 438.404 mandates that notices be in writing and explain the reasons for denial, reference the medical necessity criteria or other processes used, provide the enrollee’s rights to copies of evidence and appeal, and outline procedures for expedited review.1
In practice, this means letter templates must include:
- A clear description of the decision and the specific denial reason,
- The criteria or protocol relied upon (with member access to it free of charge),
- Instructions on how to appeal (standard and expedited),
- Rights to benefits continuation pending appeal under defined circumstances.2
Failure to incorporate these elements or to issue the notice within required timeframes can expose plans to audit findings, grievances, and regulatory penalties. The tighter the regulatory lens becomes, the less room there is for “good enough” templates. Each health plan must view letter-generation not as a clerical task but as a compliance checkpoint. And beyond the regulatory content itself, many programs require that UM notices be written in plain, accessible language at the 6th-8th grade level, to ensure members can understand their rights and the basis for a decision.
Five Friction Points Inside UM Letter Workflows
Every health plan faces variations of the same problem, but the underlying breakdowns tend to cluster around five recurring fault lines:
- Fragmented Data Sources
Critical information lives in multiple systems. UM platforms, claims engines, and policy libraries. Each transfer adds latency and the potential for mismatch.
- Template Explosion
Over time, teams accumulate hundreds of letter templates to meet overlapping state and product requirements. Maintaining these manually makes even minor updates a compliance risk.
- Human Review Dependency
Because UM letters must be clinically and legally precise, most organizations rely on multiple layers of human QA. That review process, while necessary, often adds 24–48 hours to turnaround.
- Regulatory Complexity
CMS and state requirements around adverse determination language, appeal rights, and timing create constant moving targets. Even small wording deviations can trigger audit findings.3
- Technology Gaps
Many UM systems weren’t designed for dynamic document assembly. Integrating clinical rationale, structured data, and plain-language output requires middleware or manual intervention.
Each of these friction points compounds the next, creating a cycle of rework, delay, and compliance exposure even in otherwise modernized UM environments.
Connecting the Dots: What the Delay Really Costs
The operational burden of slow UM letters goes far beyond staff productivity. It directly affects regulatory performance, provider satisfaction, and member experience.
Delayed or inconsistent notices can:
- Violate CMS and NCQA timeliness standards, exposing plans to corrective action.4
- Create confusion for providers awaiting determinations, delaying care coordination.
- Generate avoidable grievances and appeals, further burdening UM teams.
The cost is not just administrative, it’s reputational. Every late or unclear letter represents a breakdown in transparency at the very point where payers are most visible to members and regulators alike.5
Building a Smarter Letter Ecosystem
Leading plans are tackling the problem not with more templates, but with smarter orchestration.
The most effective UM letter modernization strategies share three principles:
- Structured Input, Dynamic Output: Capture decision data in structured fields early in the UM process so letters can be assembled automatically with consistent language and logic.
- Governance-Driven Templates: Centralize letter libraries under compliance governance, ensuring real-time updates to regulatory text and benefit language.
- Human-in-the-Loop Automation: Use AI-assisted generation to draft letters but retain clinical reviewer oversight for rationale and tone.
The goal isn’t to remove people, it’s to remove friction. Automation should serve precision, not replace it.
When designed correctly, next-generation letter systems can cut turnaround time by 50–70%, reduce rework, and strengthen audit readiness while making communications clearer for both providers and members.
The Bottom Line
UM letters may seem administrative, but they are where compliance, communication, and care converge. If denials are the visible output of your UM program, letters are the proof of its integrity.
For payers, the question isn’t whether letters can be automated, it’s whether they can be governed with the same rigor as the decisions they document.
At Mizzeto, we help health plans modernize UM letter workflows, integrating automation, policy governance, and compliance intelligence into one seamless ecosystem.