In utilization management (UM), few metrics speak louder—or cut deeper—than overturn rates. When a significant share of denied claims are later approved on appeal, it’s rarely just about an individual decision. It’s a reflection of something bigger: inconsistent policy interpretation, reviewer variability, documentation breakdowns, or outdated clinical criteria.
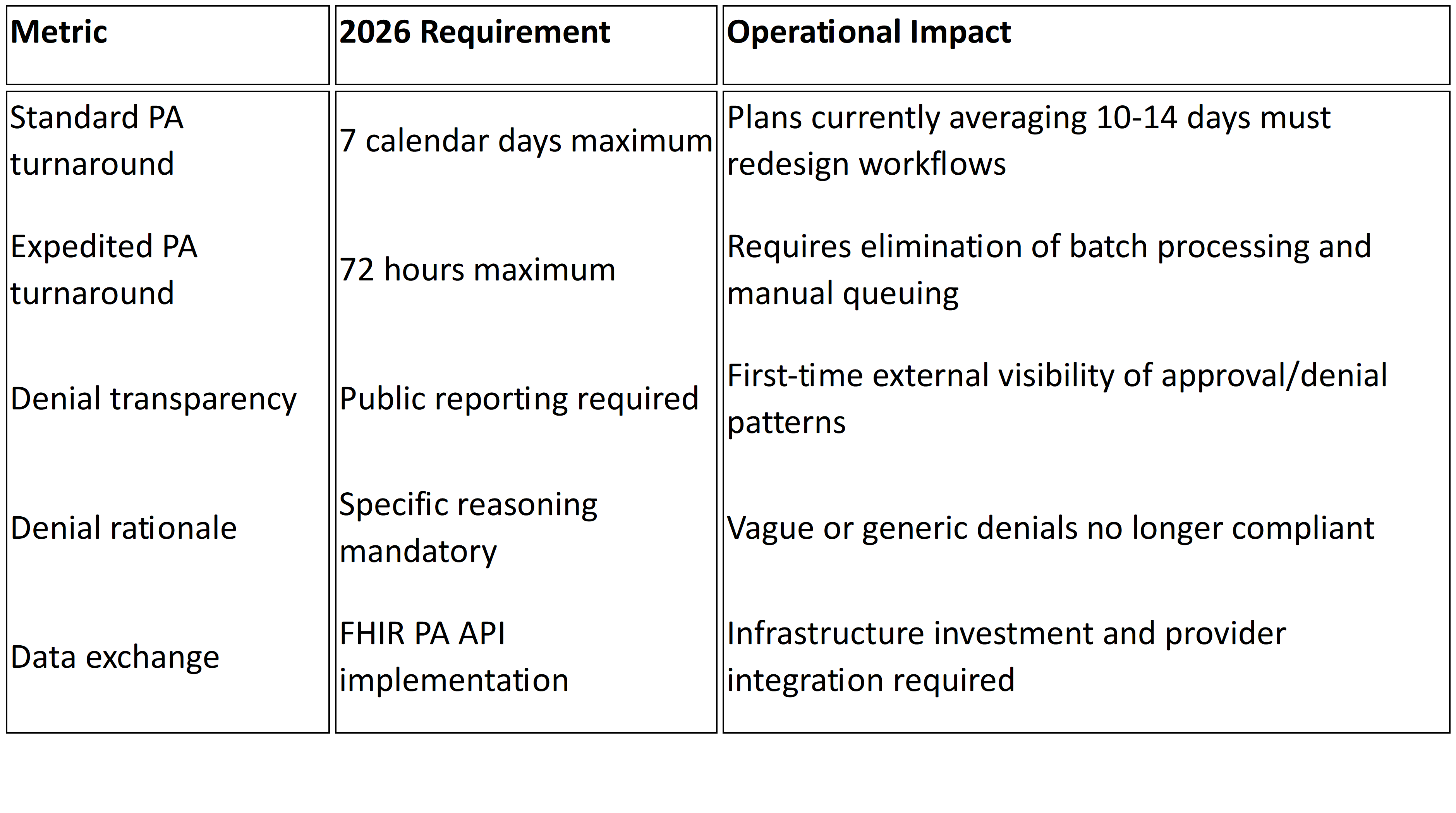
Regulators have taken notice. CMS and NCQA increasingly treat appeal outcomes as a diagnostic lens into whether a payer’s UM program is both fair and clinically grounded.1 High overturn rates now raise questions not just about accuracy, but about governance.
In Medicare Advantage alone, more than 80 % of appealed denials were overturned in 2023 — a statistic that underscores how often first-pass decisions fail to hold up under scrutiny.2 The smartest health plans have started to listen. They’re treating appeals not as administrative noise—but as signals.
What Overturned Denials Are Really Saying
Every overturned denial tells a story. It asks, implicitly: Was the original UM decision appropriate, consistent, and well-supported?
Patterns in appeal outcomes can expose weaknesses that internal audits often miss. For example:
- Repeated overturns for a single service category often signal misaligned or outdated policies.
- Overturns concentrated among certain reviewers may point to training or workflow inconsistencies.
- Successful appeals after peer-to-peer discussions often reveal documentation or communication gaps between provider and plan.
These trends mirror national data showing that many initial denials are overturned once additional clinical details are provided, highlighting communication—not medical necessity—as the core failure.3 The takeaway is simple but powerful: Appeal data is feedback—from providers, from regulators, and from your own operations—about how well your UM program is working in the real world.
The Systemic Signals Behind High Overturn Rates
When you look beyond the surface, overturned denials trace back to five systemic fault lines common across payer organizations:
- Policy Rigor vs. Flexibility
Medical necessity criteria must balance evidence-based precision with real-world adaptability. Policies written without clinical nuance—or not updated frequently enough—tend to generate denials that can’t stand up under appeal.
- Reviewer Variability
Even with clear policies, human interpretation introduces inconsistency. Differences in specialty expertise, decision fatigue, or tool usage can lead to unpredictable outcomes.
- Provider Documentation Gaps
Many initial denials are simply the result of incomplete records. When appeals are approved after additional information surfaces, the problem isn’t inappropriate care—it’s communication failure.
- Operational Friction
Lag times between intake, review, and notification can distort first-pass decisions. Data fragmentation between UM, claims, and provider portals compounds the issue.
- Weak Feedback Governance
Too often, appeal outcomes are logged but not analyzed. Mature UM programs close the loop—using overturned denials to retrain reviewers, refine policies, and target provider outreach.
Federal oversight agencies have long flagged this issue: an OIG review found that Medicare Advantage plans overturned roughly three-quarters of their own prior authorization denials, suggesting systemic review flaws and weak first-pass decision integrity.4
Turning Appeals into a Feedback Engine
Leading payers are reframing appeals from a reactive function to a proactive improvement system.
They’re building analytics that transform overturn data into actionable intelligence:
- Policy Calibration: Tracking which criteria most often lead to successful appeals reveals where policies may be too restrictive or outdated.
- Reviewer Performance: Overlaying overturn trends with reviewer data helps identify where training or peer review support is needed.
- Provider Partnership: By sharing de-identified appeal insights, plans can help provider groups strengthen documentation and pre-service submissions.
- Regulatory Readiness: Demonstrating a closed-loop feedback process strengthens NCQA compliance and positions the plan as an adaptive, learning organization.
This approach turns what was once a compliance burden into a continuous-learning advantage.
From Reversal to Reform
High overturn rates are not just a symptom—they’re an opportunity. Each reversed denial offers a data point that, aggregated and analyzed, can make UM programs more consistent, more transparent, and more clinically aligned.
The goal isn’t to eliminate appeals. It’s to make sure every appeal teaches the organization something useful—about process integrity, provider behavior, and the evolution of clinical practice.
When health plans start to see appeals as mirrors rather than metrics, UM stops being a gatekeeping exercise and becomes a governance discipline.
The Bottom Line
Overturned denials aren’t administrative noise—they’re operational intelligence. They show where your policies, people, and processes are misaligned, and where trust between payer and provider is breaking down.
For forward-thinking plans, this is the moment to reimagine UM as a learning system.
At Mizzeto, we help health plans turn appeal data into strategic insight—linking overturned-denial analytics to reviewer training, policy governance, and compliance reporting. Because in utilization management, every reversal has a lesson—and the best programs are the ones that listen.
SOURCES
- National Committee for Quality Assurance (NCQA). Overview of Proposed Updates to Utilization Management Accreditation 2026
- Kaiser Family Foundation (KFF). “Nearly 50 Million Prior Authorization Requests Were Sent to Medicare Advantage Insurers in 2023"
- American Medical Association (AMA). “Prior Authorization Denials Up Big in Medicare Advantage"
- U.S. Department of Health & Human Services, Office of Inspector General (OIG). Some Medicare Advantage Organization Denials of Prior Authorization Requests Raise Concerns About Beneficiary Access to Medically Necessary Care